“Make everything as simple as possible, but not simpler. ”
– Albert Einstein –
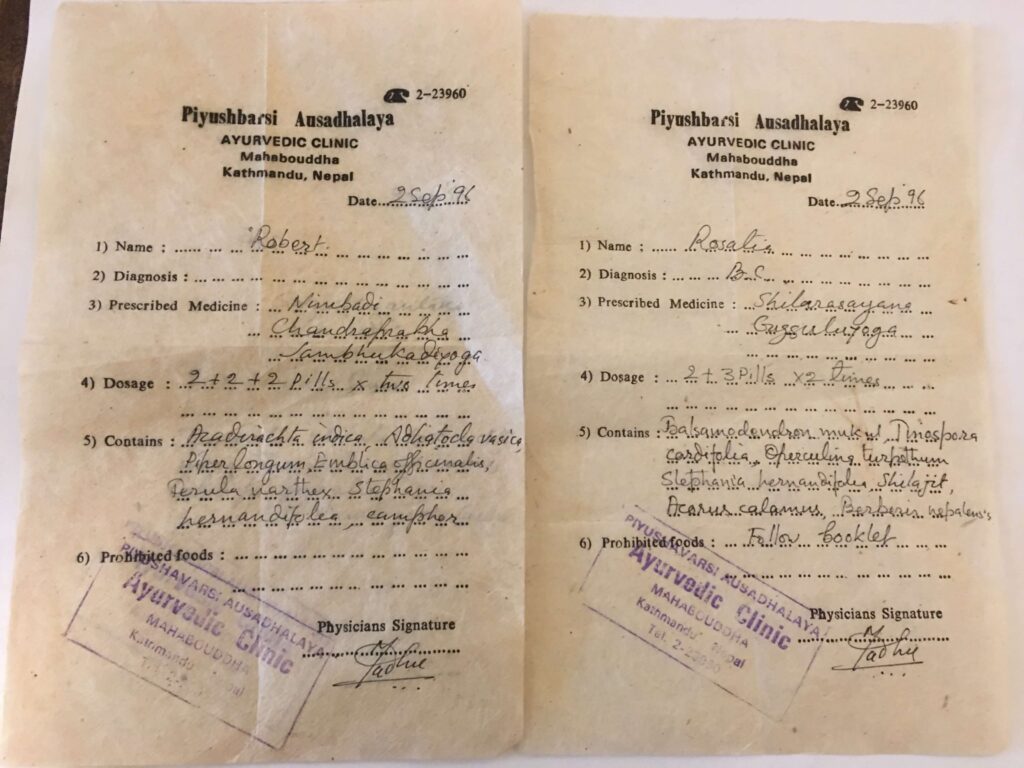
The key thing Nai-shing and I do every day is to formulate treatment protocols specific to the individual needs of the patients we see. In this section I want to show you how we go about putting our knowledge to use in the clinic. I want you to understand how herbalists throughout the world can solve real medical problems with scientific reliability. To do that, it was necessary for me to give you background information and basic vocabulary.
In the first sections of this teaching website I covered the basic herbal traditions, herb growth and preparation, safety issues, and some essential language tools. In the second section I introduced you to about 100 of the most important and trusted herbs my wife and I use at our acupuncture and herbal medical clinic in Delaware. This section is a little bit more technical, but now you are prepared to understand it. Congratulations. Let’s begin.
First of all, to treat real diseases, it is not enough to know what the individual herbs do. You must also incorporate diagnostic information, physiological knowledge, problem-solving skills and guiding philosophical principles. We will explore a few of the main diagnostic and conceptual tools used by the three different medical systems I work with, all the while recognizing that we are navigating just the smallest tributary of the herbal sea.
It took me quite a while to figure out how I could simplify the vast amount of information required to deal with the complexities of medical treatment. Then I recalled to story my friend molecular biologist Jon Narita told me about how biochemists learn. Rather than attempting the impossible task of learning absolutely everything there is to know about the biochemical life processes, they choose a few key areas of biochemisty to study in depth. This gives them the essential background to understand other areas as needed. We will do the same here, as we examine some facets of our major herbal traditions.
• Our discussion of TCM will explore some of the concepts regarding causative factors, which are clinically very useful, and are simple enough to begin to apply right away
• Our discussion of Western medicine will examine blood testing, a practice of great value in understanding your health that is often confusing to patients.
• Our discussion of Ayurveda will explore some philosophical issues to try to understand how these ancient truths still have relevance and value in modern medicine. I will go out on a limb here, and reveal some evidence that may shock you into seeing the world in a different light.
• We will also examine some integrated concepts, including a simplified tongue and pulse diagnosis system appropriate for beginning and intermediate students.
How to Construct Herbal Solutions to Health Problems
When you are ready for herbal treatment, whether for yourself or for others, the first step you must take is to objectively examine the health and identify problem areas. Most people could stand to make at least a few dietary and lifestyle changes to improve their health. Once you have identified the areas that need improvement, you can begin to develop a treatment protocol. Remember that you can always make adjustments along the way as you figure out which therapies and/or regimens are appropriate.
When it comes to the world of herbal therapy there are several levels of knowledge and expertise, beginning with the novice and ending with the skilled practitioner. It is important to identify your level so you know how to proceed.
• Level 1: Rank beginner.
If you are completely clueless, but smart enough to know that you don’t know, the best thing you can do is find a good natural medicine therapist and do as you are told. You should ask around and do some research on your own before choosing a practitioner. It’s always a good idea to explore your options, and it helps to get recommendations from people you trust. After working with a good herbal practitioner your understanding will mature. See the resource guide for information on how to locate a practitioner.
• Level 2: Educated consumer. If you have already educated yourself in the basics of holistic medicine, you may want to get a good diagnosis from your doctor and research over-the-counter treatments as well. Once you are familiar with all the available options, you can make a choice whether to see a professional or begin to develop your own herbal protocol using the guidelines I’ve provided. If you have completed this book you will be better equipped to sort through the wealth of information out there. Don’t fall into the trap of using everything that is “good for the liver” or “good for diabetes.”
Most of the herbs I list are readily available in the consumer marketplace, but you may have difficulty tracking down a select few. If you’re not sure how to obtain some of the herbs and preparations I’ve discussed, refer to the resource guide at the end of the book—you may find the answers there. If not, ask the manager or owner of your local natural foods store.
I would suggest starting slowly, incorporating just a few well-chosen single herbal or nutritional products along with the necessary and appropriate lifestyle changes. Depending on the results you want to achieve, it is possible that a combination product or formula already exists for your particular needs. Write out a list of the herbs I have recommended for your particular needs, and take it with you to the store. You may find a pre-packaged formula (tincture or pills) that contains at least some, if not all of the herbs you’re looking for. Always remain aware of your limitations, and do not hesitate to seek out professional help if the problem is more complicated.
• Level 3: Budding herbalist.
If you are a budding herbalist, you are not only self-educated, but may also have amassed a solid base of experience using various herbal medicine therapies. You may not feel limited to pills and capsules. You may want to try combining a group of herbs in a formula after studying each one carefully. This will require you to find sources for some of the more exotic Chinese and Ayurvedic herbs. (Sources for most of the herbs I use can be found at one of the locations listed in the resource guide.) It is important to note that the herbs may not all be available in the same form, so be creative. If you compile a list of ten herbs you want to use, and find that seven are available as crude powders and three as tinctures, it may be necessary to make a tea from the crude herbs and add the tinctures to the tea before drinking. Also, recognize that you will have to defer to qualified health care practitioners for serious or difficult problems. Don’t trick yourself into thinking you can treat nephritis compounded by liver disease at home.
• Level 4: Skilled therapist or physician.
If you are a skilled therapist or physician looking for solutions to health problems faced by your patients, you may recognize the inherent difficulties in trying to match herbs with patients in the real world. You probably already have good sources for herbal materials and utilize a system of clinical and differential diagnosis. Either you have already explored the patient’s health condition and understand the underlying causative factors, or you’re in the process of working this out. At this point you can read about my personal approach to each specific disease process and take note of the herbs I recommend for treatment. Then you can do your own supplemental research to identify and utilize only those herbs that match your patient’s particular needs. Additionally, skilled practitioners entering from a scientific discipline background must recognize the philosophical requirements of herbal medicine. You must be aware of and sensitive to your patients’ emotional and spiritual needs in addition to their physical and dietary requirements. Herbal medicine is more than herbs. But, I’ll bet you already knew that.
Please note that within the discussion of each disease, I have identified important causative factors, as well as possible herb choices if those factors are relevant in a particular case.
DIAGNOSIS
Signs, Symptoms & Specifics of Classification and Diagnosis
The general public is most accustomed to approaching health conditions by diagnostic category or name, such as asthma, diabetes or arthritis. This is often the standard approach of Western medicine, and it is important. In fact, a specific and clear diagnosis based upon physiology is very, very important. If someone has eye pain, for example, it is important to make sure a hidden tumor or chemical poisoning is not the cause.
However, although diagnostic terms offer us important information about the problem, oftentimes it is not enough to determine the proper herbal treatment. In fact, although we do not usually see it, each of us is bound by often-unexamined beliefs about the nature and meaning of disease drawn from our culture and upbringing.
For example, a diagnosis of asthma seems to clearly tell us that the patient has trouble breathing. We assume that this word means something specific. In fact, it does not tell us the level of inflammation in the lungs, the amount of mucus in the lungs, the amount of tension in the surrounding muscles, the level of diaphragm use or disuse, or anything about contributing causes such as exposure to toxins or cigarette smoke. Therefore, you cannot simply take “asthma” herbs and expect good results.
To understand how an herbalist or trained holistic doctor thinks, you must first recognize that diseases can be examined, diagnosed and treated from different points of view. When a practitioner draws ideas from a system of thought, whether Western, Naturopathic, Ayurvedic or Chinese, we say the prescribed treatment is based upon signs and symptoms.
We define a symptom as any departure from normal structure, function or sensation experienced by the patient. The most important part of this definition is the phrase, “experienced by the patient.” We define a sign as a change in the normal structure or function of the body that can be discovered by examination. The focus of this definition is the idea that a sign is “discoverable by examination.” Symptoms are subjective, while signs are objective and usually more physiologically specific. Symptoms and signs do not quantify the disease. Rather, they should lead to an accurate understanding of the underlying cause.
Natural Medicine Understanding of Causative Factors
In Western medicine, causation is related to morbid changes in the biochemical or physical structure and function of the body. Determining the cause requires data collection (urine, stool, images, subjective and objective findings etc.) and systematic comparison and contrast of the findings until you can determine a specific diagnosis.
In TCM, causation (bing yin) is related to “patterns of imbalance” which are discovered by the signs and symptoms as understood in this system. Determining the pattern requires a questioning process along with pulse and tongue observation to define the nature or mechanism of the imbalance (i.e. deficient, excess, cold, hot, wind), and the location (i.e. internal organs, blood, energy meridians) of the imbalance.
In TAM, causation (hetu) is related to aggravating agents (foods, behaviors, emotional changes, seasonal influences, physical injuries etc.) that cause either direct physical damage, or an imbalance in Vata, Pitta and/or Kapha which leads to the emergence of doshas (pathogenic defects). Determining the imbalance requires questioning, observation and testing to define the prognosis, symptoms and morbid anatomy. Diseases are defined both by specific name (as in Western medicine) and by the nature and location of the doshas.
Understanding the TCM Causative Factors
TCM doctors use several basic ideas beyond Yin, Yang and Qi (discussed here) to assist in their diagnoses and herb choices. As I mentioned earlier, these terms are effectively used to describe the external world we live in, as well as conditions that can penetrate and reside in the body.
“Deficiency” and “Excess” are basic TCM medical terms. In diseases of deficiency, there is a pre-existing weakness in the tissues or immune system that creates a hypersensitivity to normal conditions. In excess conditions, the disease is due to causative factors like stress or toxins that congest or overcome normal resistance.
For example, a high cholesterol level is a disease of deficiency if caused by a weak thyroid (which slows down the metabolism). Conversely, the same condition is a disease of excess if caused by a dietary excess of poor quality fats.
One well-known health problem that can help us understand how deficiency can cause what appears to be a fever-like condition are the hot flashes that often accompany menopause. Everyone recognizes that you cannot effectively use anti-inflammatory Western medicines or strongly cooling herbs to stop hot flashes. This is a deficiency problem—it is actually the hormonal decreases occurring during menopause, which creates this problem. Hence, it is necessary to use estrogen replacements or herbs that supplement and nourish the deficiency
The different way each person’s body responds to illness has important implications for diagnosis and treatment. For example, just because two patients suffer from hypertension doesn’t mean you can prescribe the same herbs to treat both of them. If one is a 96-pound 80-year-old grandmother, and the other looks like Arnold Schwarzenegger, you obviously need to account for differences in their body size, strength and general state of health before recommending a treatment.
• Diseases of deficiency are usually treated with nourishing tonics.
• Diseases of excess are usually treated with herbs that remove the excess or which stimulate the excretory organs to do so.
Note: Yang diseases tend to be external, excessive, hot and dry in nature. Yin diseases tend to be internal, deficient, cold and damp in nature.
The concepts of heat and cold have already been described in terms of the herbal energetics, or the actions of herbs. Some herbs are described as heating and some as cooling.
Similarly, diseases can be hot (inflammatory) and hypermetabolic in nature, or cold and hypometabolic. TCM doctors explain the difference between internal and external heat and cold.
External heat results from an influence outside of the body, as when the skin is inflamed by the sun. Internal heat results from internal disturbance, fever or toxins. External cold results from an outside influence, as when the body gets chilled due to low air temperature. Internal cold results from a metabolic weakness inside the body, as when the thyroid is underactive.
• Hot conditions are treated with cooling herbs
• Cold conditions are treated with warming herbs.
“Dampness” refers to an accumulation of fluids in the body. When the dampness resides in the outer muscles and tissues, you feel stiff and swollen, often with dull pain and edema. If the dampness resides in the digestive system, you might feel nausea and sluggish digestion. If the dampness resides in the lungs, you will feel heaviness and air hunger.
Dampness has three basic levels in Chinese thinking, starting as simple fluid accumulation, progressing to thicker partially congealed dampness, and leading later to thicker viscous accumulations of mucus.
• Dampness is treated with herbs that remove dampness or break up mucus, or herbs that increase metabolism to drive out the dampness. TCM doctors also use herbs that stimulate Qi to drive out the dampness.
Dryness” is the opposite of dampness, and can be caused when heat and inflammation dry out the bodily fluids, or when blood supply to the tissue(s) is poor.
• Dryness is treated with herbs that moisten, or herbs that nourish the blood.
“Wind” refers to disturbances of the nervous system, which result in symptoms like spasms, paralysis, dizziness, shaking, convulsions and nervous tension and/or irregular functioning in individual organs or systems.
Pains or tensions that quickly move from one area to another are also attributed to wind by TCM doctors, as well as certain skin and liver problems. TAM doctors look for signs of gas or swelling in tissues or in the abdomen that yield to external pressure and bounce back.
These ideas show that the TCM, Western and TAM conceptualization of “wind” are a bit different. I think the Ayurvedic way of approaching this is the most clear, so I use it in my practice. However–and this is important to grasp–if I am reading about or using TCM herbs, I have to defer to their understanding to fully grasp how and why they would choose a particular herb.
The same is true when I am choosing Western herbs.
• Wind is treated in TAM with herbs that calm, warm and nourish, and reduce Vata dosha and in TCM with herbs that nourish the blood, herbs that remove heat from the liver, or herbs that nourish the Liver Yin. Western herbalists treat wind with antispasmodic and nervine herbs.
Making TCM Causative Factors Real and Useful
It is easiest to understand how causative factors “exist” during most disease processes when we combine them to describe a problem. For example, if you have a fever and a chest cold with thin green phlegm, this is a heat and mucus condition. If you have a fever and a spasmodic cough, this is a wind and heat condition. I use this simple system of classification not only to help me prescribe herbs but also to aid in selecting appropriate diets during illness.
• For a spasmodic cough with fever, a TCM doctor would use herbs that remove wind and heat from the lungs.
• For knee and ankle swelling which “bounces back” when pressed, indicating trapped gas, the TAM doctor would use an appropriate swelling treatment (Kapha-reducing diuretic herbs) along with herbs that reduce Vata.
• For painful urination with a “funny smell,” a Western holistic doctor or a Naturopath would order a urinalysis to culture for infectious organisms, do blood tests to check for metabolic problems, and prescribe herbs or antibiotics based upon results.
The Importance of Scientific Diagnostics
As mystified as people are with Oriental medical concepts, I have seen just as many if not more people mystified by Western diagnostic concepts and tests. Blood tests, for example, are windows into your health, because your blood interacts with just about every cell in your body. Equally as important as any natural medicine concept, these tests are excellent ways to measure to benefits or failure of herbal treatment, providing–in conjunction with symptom changes–guidance to your caretakers.
Over the past seventy years, scientists have made tremendous progress in disease diagnosis and in our understanding of pathological processes. Good diagnostics are a vital part of holistic medicine. At our clinic we see many patients after they have received a diagnosed from Western-trained doctors, and we also send patients out to Western specialists when we find a need for further diagnosis. Oftentimes, using specific scientific diagnostics in conjunction with herbal signs and symptoms can be critically useful for choosing the correct treatment protocol, herbal or otherwise.
Today, as the study of herbs continues, we now know much more about the specific biochemical actions of herbs. Therefore, if someone has, for example, a deficiency of a particular blood component, such as platelets or red blood cells, we can choose herbs that have been shown to improve those blood parameters.
The following is a simplified explanation of the most common blood tests that your doctor may run. Good physicians will explain these tests to you, and as a patient you have the right to get copies for your own edification. Normally you will find reference ranges next to your test results in each category, so you can see if your numbers fall within normal values.
• Complete Blood Count -(CBC) This test measures the total number of red and white blood cells. It works with percentages, and analyzes them in different ways. The CBC includes a number of different tests, and measures your numbers against average values in each area to determine if they are high or low.
1. RBC test – Measures the number of red blood cells in a given volume of blood. Your red blood cells carry oxygen to your tissues. A low count of red blood cells can indicate blood loss, reduced RBC production (often due to nutritional deficiencies), or increased RBC destruction.
2. WBC test – Measures the number of white blood cells. A low white cell count can often be attributed to the same general causes as RBC’s, and may indicate immune system deficiency. An increased white count may indicate that the body is fighting an infection.
3. HGB test – Measures your RBC hemoglobin, a protein that carries oxygen and carbon dioxide. A low level of hemoglobin indicates a reduced ability to carry oxygen, which can be caused by many chemical factors such as auto fumes, toxic gases, cigarette smoke and blood loss. Elevated levels can indicate vitamin B-12 deficiency.
4. HCT test – Measures hematocrit, the proportion of RBC’s in your blood. A low hematocrit count indicates anemia, possibly due to nutritional deficiencies.
5. MCV test – Measures the average size of your RBC’s (mean corpuscular volume). The RBC’s can swell up in response to inflammation, liver disease or even abnormal production problems in the bone marrow. This increased MCV often causes them to die off faster, leading to anemia. When cells are too small (low MCV), it is often indicative of nutritional deficiencies.
• Individual White Blood Cell Tests – Segmented neutrophil test, lymphocyte test, monocyte test, eosinophil test and basophil test are all different types of WBC tests. These cells are easily depleted by infections or chemical stress, so if these numbers are low, or imbalanced with too many of one type and not enough of another, it usually indicates some type of physical or chemical stress. This phenomenon is directly related to immune system deficiency, which we will discuss in more detail in our discussion of the immune system.
• Platelet test – Platelets are small corpuscles that participate in the blood clotting process. Low numbers may indicate bone marrow or autoimmune problems. High numbers may indicate poor spleen function.
• Blood Chemistries – Blood chemistry tests look for different substances normally found in you blood serum.
Note on Cholesterol Tests (Lipid Profile): There are several different types of lipids (fats) in your blood. According to current medical theory, elevated levels may increase your risk of arteriosclerosis, stroke and heart attack. However, there are many reasons to be skeptical of these tests.
1. TC (Total cholesterol) test -This test measures the blood level of a particular lipid called cholesterol.
2. HDL (high-density lipoprotein) test – The high-density lipoprotein is a good and important fat. I tell people to remember this as “Happy DL.” If levels are low, it indicates a greater risk of cardiac artery disease. Things that can lower HDL include lowered by lack of exercise, genetic factors, and chemical drugs.
3. LDL (low-density lipoprotein) test – LDL is a bad cholesterol, which I tell patients to remember by calling it “Lousy DL.” People with LDL levels that are too high are at greater risk of developing heart disease.
4. Glucose test – This test measure the amount of sugar in your blood. Elevated levels indicate poor glycemic control or diabetes, and low levels can indicate the presence of hypoglycemia. The A1C test measures blood sugars over a several month period.
5. Triglyceride test – This test measures a type of blood fat that is usually elevated due to a dietary sugar excess.
6. Uric acid test – Uric acid is a waste product from nucleotide metabolism. Uric acid is actually an antioxidant, produced by your body in response to inflammation. High levels indicate the presence of gout or arthritis, and occasionally kidney disease or leukemia.
7. Total Protein test – Proteins are manufactured and used by your body for innumerable processes related to growth, repair and defense. Elevated levels can indicate problems in the liver, kidneys or general metabolism, while low levels often indicates nutritional deficiency conditions.
7a. Albumin test – Elevated levels of this protein relate to dehydration, while lowered levels relate to malnutrition, poor absorption, liver and kidney disease, and metastatic cancers.
7b. Globulin test – Elevated levels indicate lupus, melanoma, liver disease and sarcoidosis. Lowered levels indicate immune system deficiency.
7c. A/G ratio – This is the ratio between albumin and globulin. A lowered ratio is indicated in severe inflammation or infection, liver disease, colitis, kidney disease, diabetes, and metastatic cancers.
8. Calcium test – Calcium in your blood is necessary to maintain bone metabolism and numerous other metabolic processes. Deficiency can relate to heart palpitations, muscle spasms, bone loss or bone diseases, inflammation, vitamin D deficiency etc.
9. Inorganic phosphorus test. Elevates levels of phosphorus are found in parathyroid problems, bone and calcium metabolism problems, diabetic acidosis, and some forms of kidney disease.
10. Bilirubin total test – This test measures the ability of the liver and spleen to break down and eliminate dead red blood cells. Elevated levels indicate liver disease and certain types of anemia. 10a. Bilirubin direct – Elevated levels are related to obstructions, such as obstructive jaundice, gall stones, and tumors. 10b. Bilirubin indirect – Elevated levels indicate liver diseases, anemia, and gall bladder disease.
11. BUN (Blood urea nitrogen) test – Measures the ability of the liver and kidney to eliminate the by-products of protein metabolism. Elevated levels are seen in adrenal, liver, thyroid and anterior pituitary dysfunction. Low levels are seen in posterior pituitary dysfunction.
12. Creatinine test – Measures the ability of your kidneys to excrete a byproduct of muscle metabolism. Increased levels are seen in kidney failure, urinary obstruction, dehydration, muscle diseases and hyperthyroidism.
13. BUN/Creatinine ratio – A measure of kidney function. Elevated levels can mean kidney disease, excess protein, insufficient fluid intake, and prostate swelling (BPH).
14.Sodium test – Sodium is related to maintenance of calcium/phosphorus ratios and acid-alkaline balance. Elevated levels are related to dehydration, excess salt intake, and kidney diseases. Low levels are related to low adrenal function, heart failure, and vomiting.
15. Potassium test – Potassium is essential to heart and kidney function. Elevated levels are related to acidosis, adrenal deficiency, pharmaceutical side effects, and kidney disease. Decreased levels are found in liver cirrhosis, malnutrition, alkalosis, diarrhea, fatigue, irregular heartbeat, and kidney diseases.
16. Carbon dioxide test – CO2 levels are related to blood acid and alkaline balance. As levels rise, hemoglobin decreases leading to oxygen starvation. Elevated levels are found in lung disease and alkalosis and low levels are found acidosis, inflammation or hyperventilation.
17. Magnesium test – Magnesium is an important mineral for many metabolic processes. Low levels can indicate diarrhea, muscle or other spasms, poor nutrition, diarrhea, heart irregularity, and diabetes
18. SED rate – The sedimentation rate test measures clumping of red blood cells. It elevates when there is an infection or inflammation anywhere in the body. It does not indicate where the inflammation is, only its existence.
• Blood Enzymes – Enzyme levels in your blood act as markers for damage to various tissues. Elevated levels indicate problems in specific areas, especially with your liver.
1. LDH test – This test measures lactate dehydrogenase, an enzyme that is widely distributed in the body. Elevated levels indicate heart tissue destruction (heart attack), anemia, leukemia, malignancies, brain or muscle damage, seizure activity, and liver damage.
2. ALT (SGPT) test – This enzyme (alanine aminotransferase) is related to liver metabolism, and elevates in liver congestion, hepatitis, cirrhosis, liver cancer, severe inflammation, chemical or drug exposure, and pancreatitis.
3. AST (SGPT) test – This enzyme (aspartate aminotransferase) elevates in heart inflammation, heart attack, liver diseases, trauma, pericarditis, pancreatitis, seizures, and chemical or drug exposure.
4. Alk Phos test – This enzyme (alkaline phosphatase) measures metabolism in bone, liver and tumor cells. It elevates in prostate cancer, prostatitis, heart attack, excessive platelet destruction, and liver or bone diseases.
In our practice we use these blood tests extensively to monitor the progress of our patients. If someone has hepatitis, we monitor liver enzymes. If a patient has an immune system deficiency, we monitor the white blood cell counts. Because herbs are so effective at lowering elevated liver enzymes and raising WBC counts, this is a perfect example of the integration of systems.
Ayurveda Made Real
Vata, Pitta and Kapha in Diagnosis and Treatment
I remember attending a conference with a budding holistic MD many years ago. As I talked to him about Vata, Pitta and Kapha, I could see him growing impatient. Finally he said, “I’m trying to remain open-minded. But, frankly, I’m fed up with ethers, auras, Yin, Yang, Kapha and Qi. Let’s get real.”
I understand his dilemma. The modern mind finds these terms primitive. We feel more comfortable calling confusion “cognitive dissonance.” The word “ulcer” sounds better to us than “fire in the stomach.” However, the meaning behind the terms is our primary concern. The job of a good translator is to change the words without altering the underlying meaning, and to find ways to make unfamiliar concepts clear.
The question I want to tackle here is, “Do the Ayurvedic conceptual divisions have a basis in physical reality?” I think that they do, and this becomes clear when we change the words a bit, and examine some lesser-known areas of biology.
When we examine large patterns, necessity dictates that we lose a certain amount of detail. However, it is a mistake to think that these simplified concepts can somehow supercede the complexity of life. They cannot. They can, at the clinical level, help us find order within the complexity, and see relationships that are otherwise hidden.
In other words, we need some background before we can understand the Ayurvedic divisions as more than folklore or contrived religious concepts. My late teacher, Dr. Mana, like all Ayurvedic physicians, firmly believes that the ancient ideas are based in philosophy (actually spiritual knowledge discovered by sages) but exist in harmony with physical realities. Like TCM and Western herbology, the concepts lead to successful prescriptions and cures. Essentially, Vata, Pitta and Kapha, as well Yin, Yang and Qi are methods that allow us to examine the status of whole system homeostasis.
However, to remain truly universal, and to avoid materializing these ancient concepts, we have to consider a few more ideas. Can we find Vata, Pitta and Kapha elsewhere in the world of biology? Can these terms help us to see things that we could not see before?
Remember first that the concepts behind Vata, Pitta and Kapha describe three elemental processes or energies understood since ancient times as regulatory, destructive (transformation or energy) and creative (growth), respectively. The organism is a whole that lives in dynamic relationship to these processes, and thus itself is arguably a regulated process, and not a “thing.” In time this translates as processes of absorption, transformation and production.
For example, the eye can absorb a photon of light and transform it into a molecular cascade of reactions, which result in the production of a neural electrical impulse. The digestive system absorbs nutrients and transforms them through a different cascade into our physical structures.
The same three aspects can also be identified in the spatial organization of an embryo.
Consider that in the early stages of embryonic development, human cells divide into three primary germ layers, out of which develop:
• The entire nervous system (Vata), develops from the ectoderm.
• The metabolic heart, muscle, bone, urogenital, and vascular (blood and lymph) systems (Pitta) arise from the mesoderm.
•The nutrient absorbing digestive tract (Kapha) develops from the endoderm
All organs and cells in our body develop out of these three layers. Is it not possible to consider these three primary germ cells as progenitors of three large meta-systems that maintain a systemic integrity throughout life? What we normally consider to be organs are actually sub-systems within these three. In this way of thinking, might we consider these germ layers to be our meta-organs? Further, might they not maintain a systemic integrity throughout our life spans?
The prefixes endo, ecto and meso refer to locations. Endo means inner, ecto means outer, and meso means intermediate. As we move inwardly into the organism we see the same divisions in the form of an almost infinite hierarchy of nested compartments, all with insides, outsides and middles.
Thus, our individual cells have smaller organelles within them, such as the nucleus and the mitochondria. Some physicists believe (and offer mathematical proof) that this pattern of nesting is necessary to maintain thermodynamic and biochemical equilibrium within living organisms (Ho, 1998).
What happens if we move outward? Let’s consider the work of Wolfgang Schad, the brilliant German zoologist. (Allow the “Twilight Zone” theme song to play through your head as you read this.) In his out-of-print book Man and Mammals: Toward a Biology of Form, Schad describes how relative differences in these three primary systems explain much about mammalian physiology.
Schad notes that not only are there three primary organic systems operating within mammalian organisms, these “systems” can also be seen without, in the three largest external groupings of Western hemisphere mammals–the rodents (Vata), the carnivores (Pitta) and the ungulates (Kapha), which together comprise more than 70% of mammals in this area (Schad, 1971). (Schads work is based on the teaching of Goethe, and a brief review of how this works can be found here.)
• Vata animals – Rodent physiology (mice, squirrels, beavers etc.) emphasizes nervous system development. Small in size, they are known to have restless and highly sensitive natures.
• Kapha animals – Ungulate physiology (cows, horses, pigs, deer etc.) emphasizes digestive processes. They are large in size, with passive temperaments. The multiple stomachs of the cow constitute a striking example.
• Pitta animals – Carnivore physiology (lions, tigers, weasels etc.) emphasizes metabolic and energetic processes. Predatory and aggressive in nature, these animals epitomize energy and power.
Schad softened me up by pointing out that the horns on cows are actually teeth that have moved up (note that canines are nowhere to be found in cow dentation). He then essentially floored me when he pointed out that the tripartate divisions within and without all mammals could even be recognized within the subgroups.
Thus, within the large ungulates we have divisions into the super docile cows, the more aggressive swine, and the relatively nervous high-strung horses. And within the small nervous rodents, we have the more sensitive mice, the more docile squirrels, and more aggressive porcupines. Finally, even within the sensitive mouse group, we have the super sensitive harvest and field mice (Vata), the larger more docile hamsters (Kapha), and the obviously more aggressive rats (Pitta).
Ayurveda in Cell Biology
If my attempt to link ancient philosophy with modern science is to survive, I am obligated to prove that these basic patterns occur in other places, such as at the cellular level. It is easy to find Vata (regulation), Pitta (energy release) and Kapha (growth) in the individual cell. The nucleus, containing the master blueprint DNA, is obviously a regulatory (Vata) center. The cell membrane regulates the import and export of nutrient molecules–the raw materials for growth (Kapha). And in the cytoplasm of each cell we see the many organelles involved in a variety of energy and production processes, including hundreds of mitochondria, our ultimate energy (Pitta) source, providing cyclical energy to transform raw materials into useful ones.
When we look at cells from a structural point-of-view, we see that fatty acids (Kapha) are the major building blocks of the membranes, sugars called nucleosides are the building blocks of DNA and RNA (Vata), and the building blocks of our worker bee proteins are amino acids (Pitta). We will discuss the three main macronutrients, fats, carbohydrates and proteins in the nutrition section.
One of the hottest areas in biology is the molecular cell signaling systems. Molecules travel through the body until they reach receptor sites on cells where they bind and initiate vital cell processes. The vast majority of signaling molecules (like mammals) belong to one of three large families. The first thing to remember is that, like the sensitive mice group, all signaling molecules start off as Vata or regulatory phenomena. The question is, what happens next?
• Ion channel-linked receptors (Vata) – Stimulation of these sites alters the flow of ions, producing an electrical effect. They are the receptors that control voltage changes related to neurotransmission.
• G-protein-linked receptors (Pitta) – Stimulation of these cell membrane sites generally causes increases in energy activation, including cyclic AMP (which energizes nerve cells as one function), sugar breakdown (which increases energy production), accelerated heartbeat, and activation of cellular response to light and smells.
• Enzyme-linked receptors (Kapha) – Stimulation of these receptor sites causes activation of growth factors, proteins that regulate cell growth, proliferation and differentiation in our tissues (Albert et al., 1998).
Ayurvedic Body Types
With the background information just provided, it should now be easier torecognize and understand the existence of the three Ayurvedic body types (Prakriti in Sanskrit) as one expression of the tripartate patterns found throughout mammalian physiology.
Whether this is a physical reality or a “way of knowing” is irrelevant. My experience in learning to distinguish these body types has helped me greatly in my clinical practice. I recall that it was not easy at first. It took me more than two years to develop the ability to identify a patient’s body and energy type quickly at the time of first meeting. You can’t imagine the effect it has on a new client when you describe their basic personality traits since childhood to them in detail after knowing them for only five minutes.
• Vata types are sensitive and restless in nature, generally high in intelligence, thinner (due to weaker digestion), and prone to nervousness and fatigue when ill.
• Pitta types are aggressive and strong-willed in nature, generally hot, highly energized and physically strong (due to strong metabolism), and prone to inflammatory conditions when ill.
• Kapha types are slow and stable in nature, generally heavy and solid physically (due to strong digestion), and prone to mucus and “sluggish” conditions when ill.
General Guidelines for Herb Use Based on Ayurvedic Body Type
• Sensitive Vata types should use lower doses of herbs, and should use warming, calming and nourishing herbs.
• Strong-willed Pitta types should use higher doses of herbs and use more cooling and detoxifying herbs.
• Slow, stable Kapha types should use more warming, spicy, energizing and mucus-reducing herbs.
It is difficult to use this theory properly unless you realize that everyone contains all three within themselves, and that many people are Vata-Pitta, Vata-Kapha and Pitta-Kapha. If you are not sure of your body type, usually you can easily pick one to eliminate, and what is left is probably you.
Ayurveda in the Clinic
Dr. Mana has taken the Ayurvedic concepts further, focusing on internal regulation. He points out that each organ and system in the body has arteries, nerves and veins that regulate its health. Vata, as the regulator of movement, can be equated with nervous system control. Kapha, as regulator of creative processes, can be equated with (or seen in action within) the body’s arterial supply of nutrients. Pitta, as regulator of destructive processes, can be equated with venous drainage of fiery metabolic wastes.
These direct associations help us gain a practical clinical understanding of Ayurveda. Each organ can be discussed in terms of how well the nervous system is doing its job (Vata), whether or not the organ or body system has sufficient or excessive nutrient and fluid supply (Kapha), and whether or not it is efficiently producing energy and draining away inflammation and waste (Pitta).
Following Ayurvedic logic, destructive agents, such as unhealthy foods, germs, viruses and toxins, enter the body or are internally generated during metabolism, after which they mix with normal gases, bile and mucus. These bodily components then act as carriers for both pathogens (waste) and nutrients. When the effects of pathogens exceed the body’s ability to detoxify and excrete (through urine, feces, sweat, exhalation, etc.) they begin to overpower their carriers.
Ayurvedic doctors monitor the health of the body through careful observation of these components. Any emergence of physical symptoms or changes in the organism as a whole indicate that a corruption, blockage or alteration has occurred. For example, if the liver cannot sufficiently detoxify, then the bile becomes toxic, and inflammation or heat increases. If the digestive system cannot fully and completely excrete heavier substances, then dampness and/or mucus begin to accumulate. If the body as a whole or individual cells cannot fully, completely or properly respire, toxic gasses begin to accumulate. It is through the physical manifestation of signs and symptoms that the doctor can identify and correct the cause of the problem.
Tongue Diagnosis
The eyes may be the windows to your soul, but your tongue is the window to your digestive system. When you eat, your teeth decimate food by crunching it like giant hydraulic presses with jagged steel edges, while your tongue darts around and wallows in the food like a greased pig in mud. (Okay, okay. I was just giving you a visual to help you remember.) During its immersion in the food bath, your tongue sends signals to the digestive system about the tastes and other qualities of the food. Think of the whole system, from the tongue to the stomach, as one long, continuous membrane. As the digestive tract undergoes various changes in its state of health, these changes are physically reflected in the tongue.
The following simple observations can help you diagnose conditions that may exist in the digestive tract:
• A swollen tongue may indicate dampness.
• A dry tongue may indicate inflammation and/or dehydration.
• A redder-than-normal tongue may indicate heat and inflammation.
• A pale tongue may indicate blood deficiency or anemia.
• A blue tongue may indicate thick stagnant blood, insufficient oxygen or poor circulation. It can also be an indicator or intestinal infection.
• A small, thin tongue (as if it has shrunk) may indicate Yin (nutrient) deficiency.
• A thick white coating on the tongue may indicate mucus.
• A thin white coating may indicate cold and dampness.
• A thick, yellow greasy coating may indicate heat and dampness.
• A puffy and swollen tongue with visible tooth marks may indicate weak digestion.
• Redness around the edges of the tongue may indicate liver inflammation
• Swelling and a bluish tint of the large veins on the back of the tongue (you can see this when you curl the tongue up) may indicate blood congestion.
• A withered and quivering tongue may indicate severe deficiency and nervous exhaustion.
Note: These signs should never be taken alone as definitive diagnoses. They are pieces of information that, along with other signs and symptoms, must corroborate to form a diagnosis and treatment protocol.
Pulse Diagnosis
The pulse is another tool herbalists use to diagnose general health conditions. The same cautions I offered about tongue diagnosis apply here as well. TCM pulse diagnosis is a highly specialized skill, and takes years to develop. In Ayurveda, doctors use pulse diagnosis to assess the levels of imbalance in Vata, Pitta and Kapha. Western doctors use pulse diagnosis primarily to determine the condition of the heart.
The following simple rules may help simplify your understanding of the pulse and its diagnostic value:
• A fast pulse may indicate inflammation or fever if bounding (Pitta) or nervousness if weak (Vata).
• A slow, weak pulse may indicate Qi deficiency (energy depletion).
• A slow, strong pulse may indicate that the person has a strong heart, possibly an athlete.
• A tense or wiry pulse (like plucking a guitar string) may indicate nervous tension or energy restriction.
• A pulse floating close to the surface may indicate the early stages of an infection.
• A slow, soggy or slippery pulse (which tries to slip away from the doctor’s touch) may indicate mucus and dampness.
• A thin pulse may indicate blood deficiency
• A deep pulse (you need to push down to feel) may indicate weakness and/or deficiency.
• An intermittent or irregular pulse may indicate congestion in the heart, as well as potential hormonal or neurological imbalances.
Taste + Temperature = Action
In both TCM and TAM the combination of taste with temperature (warming or cooling) can be used to create a simple basic description of the action of an herb. For example sweet herbs are generally nourishing. A sweet herb with a warming action would therefore probably benefit conditions requiring warmth and nourishment, such as illnesses involving nervous system weakness or weight-gain and tissue regeneration.
Commonly Used Groups of Herbs
All systems of medicine group together their therapeutic agents with similar actions. In Western medicine, for example, pharmaceuticals are grouped into families, such a blood pressure lowering agents or painkillers. More than 2,000 y ears ago, the ancient Charaka Samhita divided herbs into 50 different groups. To avoid repetition, I have placed several very important commonly used herbs into groups based upon commonly needed actions. We will refer to these groups in Section Three as we explore different body systems and the illnesses that compromise them. Please note that these groups are representative and cannot be wholly complete. Also note that some herbs fall into more than one category.
Herbs that Reduce Heat and Inflammation
Boswellia gum, bromelain, bupleurum root, burdock root, dandelion, flaxseed oil, ginger root, guggul gum, heart-leaved moonseed, holy basil, isatis root and leaves, licorice root, milk thistle seeds, neem leaves, phellodendron root, raw rehmannia root, rhubarb root, sarsaparilla, scute root, turmeric root.
Herbs that Move the Blood and Remove Blood Stasis
Carthamus flower, dang gui root, myrrh gum, prickly ash bark, red clover blossoms, salvia root, millettia stem, carthamus flower, tien chi root.
Herbs that Strengthen Weak Digestion
Black pepper, bromelain, garlic bulb, ginger root, ginseng root, trikatu (3 peppers), white atractylodes rhizome, cardamom.
Herbs that Increase Vital Force and Strengthen the Immune System
American ginseng root, astragalus root, elderberry fruit, chaga mushroom, cordyceps mushroom, ginseng root, guduchi stem, maitake mushroom, reishi mushroom, shilajatu, Siberian ginseng root, amla fruit, haritaki fruit, ganoderma mushroom, shou wu root.
Herbs that Nourish the Blood and/or Strengthen the Tissues
American ginseng root, alfalfa, dang gui root, deer antler, eclipta, shou wu root, raw rehmannia, shilajatu, amla fruit, white peony root.
Poison removing Herbs (that remove and/or protect against poisons)
Amla fruit, beet root, burdock root, castor oil, licorice root, triphala, arjuna bark, dandelion root, gotu kola, guduchi stem, berries, schisandra berries, white sandalwood, turmeric root, green tea.
Nervine group (herbs that calm and/or strengthen the nerves)
Ashwaghanda root, bala, bupleurum root, ginkgo leaf, gotu kola, kava, muira puama, reishi mushroom, schisandra berry, scullcap, St. John’s wort, valerian root, white peony root, wild asparagus root, milky oat seed.
Vessel strengthening group (herbs that strengthen and detoxify the micro-vasculature)
Blueberry, gotu kola. hawthorn berry, raspberry, stoneroot, tien-chi.
Mucus reducing group (Herbs that remove thick mucus accumulations)
Black pepper, long pepper, bromelain, guggul gum, tangerine peel, turmeric root, fritillaria bulb (chuan bei mu / F. cirrhosa), arisaema (tian nan xing /A. species), trichosanthes fruit (gou lou / T. kirilowii ), acorus rhizome.
Diuretic group (Herbs that promote urination and eliminate retention of watery fluids)
Dandelion leaf, Akebia (mu tong / A. trifoliata), plantain leaf (P. ovata), capillaris (yin chen hao / Artemisia capillaris) , punarnava root (Boerhavia difusa), parsley, Grifola mushroom (zhu ling / Polyporus umbellatus ), uva ursi leaf (Arctostaphylos uva-ursi), barley water.
Dampness removing group (Herbs that remove thickened fluids from the digestive system and tissues)
Poria mushroom, tangerine peel, pinellia tuber, licorice root, prickly ash bark, oregano leaf.
Warming group (Herbs that warm the system)
Aconite, dry ginger, cinnamon bark, black pepper, long pepper, prickly ash bark.
Nutritive group (Herbs that promote weight gain)
Ashwaghanda root, dates, cashews, bala, cardamon, white atractylodes, ginseng root, dang gui root , cooked rehmannia root.
Wound healing group (herbs that promote healing of skin, vessels and tissue)
Gotu kola, tien chi root, aloe gel, turmeric root. dang gui root, astagalus root
Intestinal healing group (Herbs that soothe and heal the intestinal membranes)
Slippery elm bark, marshmallow root, licorice root, chlorophyll juice, wild asparagus root, fennel seed, peppermint leaf, flaxseed oil, kava root.
Herbal Formulas: Addition, Subtraction and Multiplication
Dr. Duke, in his excellent (and free) online Medical Botany course, says that herbs generally interact in formulas in three ways: 1. Antagonism 2. Additivity 3. Synergy
Antagonism occurs when herbs or herbal actions work in opposing ways. For example, the coldness of neem would be antagonized or neutralized by the warmth of prickly ash bark. The bitterness of coptis rhizome would be antagonized by the sweetness of licorice root. Herbalist use this idea to modify the actions of their formulas. There can of course also be specific chemical antagonisms, but these are too complex to deal with here, and there is much that we still do not know. (Some of these properties are mentioned briefly in the safety chapter.) Because individual herbs are complex mixtures of substances, antagonism that occurs when you combine two herbs is much like the result of mixing two groups of very different people. Imagine, for example, if a group of birdwatchers and a group of biologists met at a park. Chances are they would get along quite harmoniously, though individual members of each group might have conflicts. The conflicts could be much greater in number and severity in a meeting between a group of birdwatchers and a group of longshoremen. (They actually did that on the old TV show “Candid Camera.” Woody Allen went to the longshoreman’s union hall in New York and tried to get them to join his bird-watching club).
Additivity occurs when herbs simply add to each other. Mixing a group of herbs containing immune-stimulating polysaccharides (like maitake mushroom with ganoderma mushroom) is additive, as is mixing herbs that contain phytoestrogens. Mixing herbs with similar actions to get additive effects is a common herbal strategy. Most of the herbs in the groups mentioned below have additive effects.
Synergy is a result of the combination of two or more substances that cannot be predicted by simply adding the sum of the parts. Following this phenomenon, individual nutrients must work together for the body to produces its immune response. For example, your body needs less vitamin C if you are getting adequate levels of vitamin E, because these two antioxidants support the regeneration of one another in the body (Thomas et al., 1992). Herbs like shilajatu and American ginseng root seem to generally increase and add to the actions of other herbs.
Herbal Medicine Doses – Dosage is as Dosage Does
It’s also important to know that the same nutrients can affect your body in very different ways depending on the dose. It is well known that individual herbs can act differently depending on dose. For example, ginseng extracts cause vasoconstriction in small doses, and vasodilation in large doses (Huang, 1999).
The same thing is true of individual nutrients, such as vitamin K. While low doses of this vitamin assist blood clotting, high doses (above 1 mg/day) aid calcification of the bone matrix (Seyama et al., 1996). Another case in point is vitamin C. At low doses, vitamin C aids in the generation of collagen and elastin, which help keep the body “glued together.”
At higher doses, however, ascorbic acid becomes a potent anti-viral and antioxidant compound. A final example is niacin, an important B vitamin. At low doses, niacin provides the body with adequate energy metabolism through the action of nicotinamide adenine dinucleotide (NAD). At somewhat higher doses, niacin becomes a valuable vasodilator. When the dosage is increased even more, this vitamin is a potent hypocholesterolemic (cholesterol-lowering) agent (with some dangers).
Niacin was the first drug used in the treatment of high cholesterol (Crouse, 1996).
Most of what we know about how herbs interact with each other is based on empirical knowledge. The understanding of how to combine herbs together to improve, modify or potentiate their effects is part of all mature herbal traditions. The TCM use of licorice root to “harmonize” formulas, and the TAM combination of three fruits (triphala) to create a balanced tonic effect are two obvious examples.
In fact, because each of the individual tonic fruits in triphala work a bit more on Vata, Pitta and Kapha, this is an excellent example of a well-constructed formula. The areas of antagonism, additivity, synergy and dosage are exciting ones for the future of herbal medicine. Because this research leads to a different direction than looking for single active ingredients, it is more in harmony with the philosophy of herbal medicine.
In addition to the fact that herbs and nutrients can work together or in opposition is the fact that all of us can react differently to just about everything, a concept called biological or biochemical individuality (Burgio, 1994, Rosenberg and Rosenberg, 1998). This means that no matter how much we try to standardize treatments (one size fits all), some of us simply will not respond. I think we can never get rid of the need for good doctor-patient relationship with frequent feedback leading to individualized treatments based upon personal needs.
I Still Don’t Get the Big Picture
Okay, I lied. Herbology is not that simple. Now that I’ve confused you completely, let’s see if I can sum it all up. The central goal of herbal treatment is to restore the body to balance. At a global level, the nervous system and the mind works in concert with digestive, cardiovascular and circulatory systems to regulate bodily function and health.
As I view it, these systems derive from three primary germinal layers, elemental tissues that form in the earliest stages of embryonic development. The tissue layers are called ectoderm, mesoderm and endoderm, and serve as the precursors to all tissue development. The large tube that extends from mouth to anus, forming our digestive tract and all its related organs, grows out of the endoderm tissue layer. The heart, blood vessels, connective tissue, glandular system, muscles and bones all derive from the mesoderm layer. Finally, the brain and nervous system are composed of endoderm tissue.
These three primary germ layers have evolved together; they are neither separate nor individual; they are entwined and inter-dependent, and this complexity reaches all the way down to the cellular level. For example, cell biologists have shown us that each cell in the body has its own musculoskeletal system, consisting of a stiffened skeleton composed of tubules, which are surrounded by a contractile fibrous substance.
Each aspect of the living web-like matrix of energies and systems we call the human body is designed to break down and absorb different forms of energy, which it then converts and releases outward in a never-ending flow as we move through the world.
For example, the food that we eat contains: • essential nutrients that it cannot produce itself from smaller building block • energy trapped in chemical bonds the molecules that make up food • building blocks (such as amino acids) that our bodies can use
Our digestive systems break down food into component molecules and absorbs them. The blood takes these molecules to the cells where they are used as raw materials to produce our own molecules and/or further broken down to release the energy trapped in the chemical bonds. This energy release can only be done in the presence of oxygen, and our breathing changes to accommodate ever-changing metabolic needs.
This process creates waste products that are expelled from the body via exhalation and our eliminative organs. As we move through the world, our nervous system “hears” internal signals (like hunger) and responds, perhaps by looking for food. Likewise, our cells are constantly hearing and responding to messages from the outside as well as sending signals outward. This same process (flow of energy) takes place on many levels.
The goal of this energy flow is a constant movement toward balance among all organs and systems. Health is optimal when the major systems are individually and collectively in balance. When your body is in a state of optimal health, you experience such feelings as love, peace, harmony and appreciation. Conversely, imbalances in health usually lead to emotional states of pain, fear, depression and anger. When health breaks down, certain large causative factor can be seen, including inflammation, nutritional deficiencies and regulatory dysfunction.
This is why as an herbalist, I am primarily concerned (at the physical level) with a patient’s digestive energy, circulatory and metabolic efficiency, and nervous system function. Once these primary regulators are brought back into balance, we can begin to restore a patient to optimal health. One way to do this is to use herbs.
Herbal Formula Writing Made Simple
Once you have good diagnostic information and a clear picture of your larger goals, you are ready to choose your herbs. We all understand what a good recipe is with regards to taste, texture, aroma, nutrition etc. Putting together an herbal formula is like writing a recipe.
However, there is an important intermediate step, which is stipulating a strategy. A strategy includes what you want to do to the body, the methods you choose to employ, and the order in which you want to deploy your tools.
You have seen in section two that herbs are often described by “What they do” to the body, as well as their effects on specific disease processes. This method of understanding herbs allows us to understand how to employ herbs.
Examples of simple strategies are:
• To nourish the blood
• To calm spasms in the legs
• To reduce inflammation in the liver
• To improve white blood cell counts
The above strategies are the result of diagnostic work. We would only choose herbs that nourish the blood, for example, if the person had anemia or another blood deficiency problem. So, a more complete description of the strategies mentioned above would be:
• My patient is fatigued and anemic, so I will nourish their blood.
• My patient is having painful leg spasms, to I will calm the spasms.
• My patient is fatigued and jaundiced, so I will reduce inflammation in their liver.
• My patient is undergoing chemotherapy, so I will improve white blood cell counts.
Most patients will have other secondary considerations. They may have blood sugar problems, or poor digestion, nervousness or constipation. In writing your formula, you would want to add some herbs to address these important secondary elements. This would translate the above examples into complex strategies as follows:
• My patient is fatigued and anemic due to stress and overwork, so I will nourish their blood and add some calming nervine herbs.
• My patient is having painful leg spasms due to poor absorption and poor diet, so I will calm the spasms, increase their intake of mineral rich vegetables, and add some digestive herbs.
• My patient is fatigued and jaundiced due to hepatitis, so I will reduce inflammation in their liver, council them on the importance of stopping alcohol abuse, flush the bile out with diuretics and an increase in water intake, and add some anti-viral and immune-stimulating herbs.
• My patient is undergoing chemotherapy, and white blood cell counts have decreased, especially macrophages. The gastrointestinal system is also severely inflamed. Therefore I will nourish the blood with tonics, emphasizing herbs than increase macrophage counts, and I will protect the gastrointestinal system with herbs that coat the intestinal membrane and counteract inflammation.
If you can train your mind to formulate your medical ideas in this manner, you can develop your own strategies and begin to think like an herbalist. Once you have identified the appropriate herbs and strategy for treating all aspects of the patient’s condition, you can construct your starting formula.
It helps to know that it has been a principle of TCM since its earliest classic text (Herbal Classic of the Divine Plowman, first recorded on paper over 2,000 years ago) that most basic prescriptions contain one or two major herbs, along with several supportive ones to improve activity and reduce adverse effects (Huang, 1999).
Dosage & Process: Healing with Herbs is like Playing Football
I heard a group of NFL football players on TV discussing how they sized up an opponent. I was surprised to learn that these professionals did not only look for obvious qualities like strength, size, speed and agility. They were equally concerned with knee flexibility, grip strength and peripheral vision. As explained, the latter information was necessary to determine when an opponent was coming at you from behind.
My point is that good diagnosis and treatment in herbal medicine involves noticing things that others ignore. The starting formula (and starting dosage) is like the first play in a football game. The goal is total health. The symptoms and disease states are like the opposing team. After you make your first play (write your starting formula), you have to evaluate results, then re-strategize and reformulate your secondary formula and dosages. This is like the football huddle before the second play.
In both China and Nepal, formulas are usually changed every three to five days. As the problems begin to resolve or stabilize there are longer periods of time between formula changes. Thus, good herbal medicine is an ongoing feedback process, requiring a willingness to continually change tactics.
